Non-invasive DNA screening test for early detection of colorectal cancer
Mayo Clinic and Exact Sciences, Inc. have worked together to develop a non-invasive stool DNA screening test that can detect with high accuracy early-stage malignancies and precancerous tumors (adenomas) leading to an earlier identification of colorectal cancer.
Two studies have investigated this DNA screening test and the results will be published in Gastroenterology and Clinical Gastroenterology and Hepatology.
The Mayo Clinic has licensed intellectual property to and is a minor equity investor in Exact Sciences. Dr. David Ahlquist is one of the inventors and a scientific adviser to Exact Sciences.
Stool DNA tests target multiple markers to achieve high detection rates (DNA changes may differ between colorectal cancers) and very sensitive tests are required (DNA markers may be present in only trace quantities in stool).
This type of test has been shown to be more effective than fecal occult blood tests at detecting colon cancer and precancerous polyps.
The first study was a large blinded investigation and found out that stool DNA test detects with accuracy multiple markers for colorectal cancer. Among 400 people it detected 87 percent of curable-stage cancers and the test identified most of large precancerous polyps. It has a good sensitivity and could detect 64% of polyps larger than 1 centimeter (cm); 77% of polyps larger than 2 cm; and 92% of polyps larger than 4 cm.
The second study compared a plasma test for methylated Septin 9 (SEPT9) and the stool DNA test. SEPT9 detected 14 percent and the stool DNA test identified 82% of precancerous polyps. SEPT9’s detected 60% of cancers at any stage, while the stool DNA test identified 87%. SEPT9 identified 50% of curable stage (stage I-III) cancers and the stool DNA test detected 91%. SEPT9 had 27% false-positives results and the DNA stool test had 7%.
A false-positive result is a positive test for cancer when there is no cancer. The presence of tumors above the colon (intestinal, gastric cancers) or a problem with the test may lead to false-positive results. When the stool DNA test result is positive but a follow-up colonoscopy is normal, the doctor recommends evaluation of upper gastrointestinal tract, another stool DNA test, or another colonoscopy or a combination of these.
“Cancerous and pre-cancer cells are shed into the stool and detected by the stool DNA test long before tumors progress to invade the bloodstream for later detection by the plasma SEPT9 screening test,” said David Ahlquist, M.D., of Mayo Clinic, principal investigator of both studies.
“Along with its high accuracy, this test approach could improve participation rates due to its patient-friendly features… The test is non-invasive; requires no bowel preparation, medication restriction, or diet change; and can be performed on mailed-in samples without the need, expense, or inconvenience of a health care visit,” said Dr. David Ahlquist in a news release by the Mayo Clinic.
“This test appears to uniquely represent an accurate noninvasive approach to large polyp detection, which offers the promise of actually preventing cancers from developing,” said Stephen Thibodeau, Ph.D., genetics researcher at Mayo Clinic, co-investigator.
Colorectal cancer (bowel cancer) is an uncontrolled malignant growth of the glands of the colon, appendix, rectum (cancer of the anus is a separate entity).
The majority if colorectal cancers develops over a long period (years). They start from small benign growths, polyps or adenomas.
Common symptoms are worsening constipation, rectal bleeding (blood in the stool), anemia, weight loss, fever, changes in bowel habits, loss of appetite, nausea, vomiting. If the person is over 50, these signs are very alarming.
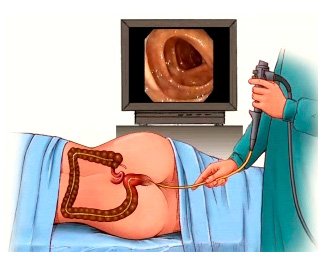
Fecal occult blood testing, flexible sigmoidoscopy and colonoscopy are the three main screening tests for colorectal cancer. The stool DNA test is a method to detect precancerous polyps and colorectal cancers in the early stages.
It is recommended that every person to start undergoing colonoscopy at the age of 50 for colorectal cancer screening and to continue it until the age of 75 (sigmoidoscopy every 5 years and colonoscopy every 10 years). Unfortunately, this is often ignored and the disease is identified at later, severe stages.
Older age, male gender and heredity are the risk factors for colorectal cancer that cannot be changed. However, obesity, red meat, a high fat or high alcohol intake (more than a drink per day) can be controlled. As well as smoking and a lack of physical exercise.
Increasing the consumption of whole grains, fruits and vegetables, and reducing the intake of red meat are recommended for colorectal cancer prevention. Physical activity can moderately reduce the risk of colorectal cancer.
Apparently the acetylsalicylic acid (aspirin) and celecoxib decrease the risk of colorectal cancer in those at high risk, but they are not recommended in those at average risk. While vitamin D intake and blood levels are associated with a lower risk of colorectal cancer, there was some evidence for calcium supplementation but it is not sufficient to make a recommendation.
According to the American Cancer Society the lifetime risk of developing colorectal cancer is one out of every twenty Americans. This there will be over 140,000 new cases of colorectal cancer, and around 50,000 deaths, it is estimated.
