Home Tags Posts tagged with "dementia"
dementia
Experts from Edinburgh University found that exercising in your 70’s may stop your brain from shrinking and showing the signs of ageing linked to dementia.
Brain scans of 638 people past the age of retirement showed those who were most physically active had less brain shrinkage over a three-year period.
Exercise did not have to be strenuous – going for a walk several times a week sufficed, the journal Neurology says.
But giving the mind a workout by doing a tricky crossword had little impact.
The study found no real brain-size benefit from mentally challenging activities, such as reading a book, or other pastimes such as socializing with friends and family.
When the researchers examined the brain’s white matter – the wiring that transmits messages round the brain – they found that the people over the age of 70 who were more physically active had fewer damaged areas than those who did little exercise.
And they had more grey matter – the parts of the brain where the messages originate.
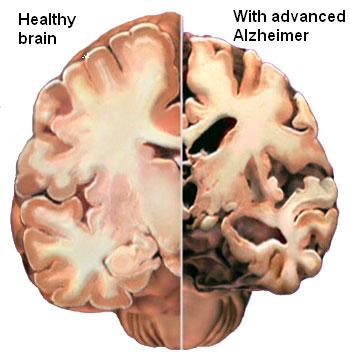
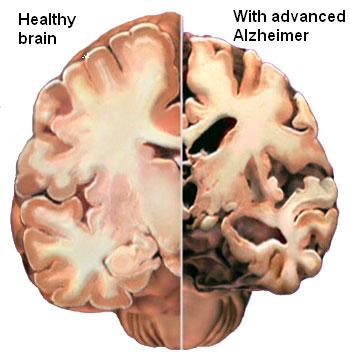
Experts already know that our brains tend to shrink as we age and that this shrinkage is linked to poorer memory and thinking.
And previous studies have shown that exercise helps reduce the risk of dementia and can slow down its onset.
But scientists are still baffled about why this is.
Exercise increases blood flow to the brain, delivering oxygen and nutrients to brain cells, which may be important.
Or it may be that as people’s brains shrink, they become less inclined to exercise.
Regardless of why, experts say the findings are good news because exercise is an easy thing to do to boost health.
Prof. James Goodwin, head of research at Age UK, the charity that provided the funding for the research, said: “This research re-emphasizes that it really is never too late to benefit from exercise, so whether it’s a brisk walk to the shops, gardening or competing in a fun run it is crucial that, those of us who can, get active as we grow older.”
A new research has find that an aspirin a day may slow brain decline in elderly women at high risk of cardiovascular disease.
Around 500 at risk women, between the ages of 70 to 92, were tracked for five years – their mental capacity was tested at the start and end of the study.
Those taking aspirin for the entire period saw their test scores fall much less than those who had not.
The Swedish study is reported in the journal BMJ Open.
Dr. Silke Kern, one of paper’s authors, said: “Unlike other countries – Sweden is unique, it is not routine to treat women at high risk of heart disease and stroke with aspirin. This meant we had a good group for comparison.”
The women were tested using a mini mental state exam (MMSE) – this tests intellectual capacity and includes orientation questions like, “what is today’s date?”, “where are we today?” and visual-spatial tests like drawing two interlinking pentagons.
But the report found that while aspirin may slow changes in cognitive ability in women at high risk of a heart attack or stroke, it made no difference to the rate at which the women developed dementia – which was also examined for by a neuropsychiatrist.
Dr. Silke Kern added: “We don’t know the long term risks of taking routine aspirin. For examples ulcers and serious bleeds may outweigh the benefits we have seen. More work is needed. We will be following up the women in this study again in five years.”
Being overweight is not just bad for your waistline but for your brain too, say researchers who have linked obesity to declining mental performance.
Experts are not sure why this might be, but say metabolic changes such as high blood sugar and raised cholesterol are likely to be involved.
Obesity has already been tipped as a risk factor for dementia.
The work, published in Neurology, tracked the health of more than 6,000 British people over a decade.
The participants, who were aged between 35 and 55, took tests on memory and other cognitive skills three times over a 10-year period.
People who were both obese and who had unhealthy metabolic changes showed a much faster decline on their cognitive test scores compared to others in the study.

Being overweight is not just bad for your waistline but for your brain too
The experts stress that they only looked at cognitive function, not dementia.
The boundary between normal ageing, mild cognitive impairment and dementia is blurred – not all impairment leads to dementia.
All of the study participants came from one group of civil service workers, which may mean the findings may not apply more generally to other populations.
They said: “More research is needed to look at the effects of genetic factors and also to take into account how long people have been obese and how long they have had these metabolic risk factors and also to look at cognitive test scores spanning adulthood to give us a better understanding of the link between obesity and cognitive function, such as thinking, reasoning and memory.”
Shirley Cramer of the Alzheimer’s Research UK said: “We do not yet know why obesity and metabolic abnormality are linked to poorer brain performance, but with obesity levels on the rise, it will be important to delve a little deeper into this association.
“While the study itself focuses on cognitive decline, previous research suggests that a healthy diet, regular exercise, not smoking and controlling blood pressure and cholesterol in midlife can also help stave off dementia. With dementia figures spiralling towards a million, the findings suggest we should be conscious of our general health throughout life.”
US pharmaceutical companies Pfizer and Johnson & Johnson say they will stop development of Alzheimer’s drug bapineuzumab, because it failed in two late-stage clinical trials.
Bapineuzumab, made by Pfizer and Johnson & Johnson, was designed to halt build-up of plaque in the brain.
But it failed to improve cognitive or functional performance compared with a placebo in certain patients.
Alzheimer’s is the most common form of dementia, as well as the sixth leading cause of death in the United States.
An estimated 36 million people worldwide are believed to have dementia, including Alzheimer’s.

Bapineuzumab, made by Pfizer and Johnson & Johnson, was designed to halt build-up of plaque in the brain
Both firms announced on 23 July that the first clinical trial of the intravenous (IV) version of bapineuzumab had failed.
In that study, patients with a gene that is associated with a greater risk of Alzheimer’s were tested.
But results with the group were largely the same as with those who did not have the gene, who were tested in the second study.
The second trial’s end means that additional studies on the IV version will not take place; however, Johnson and Johnson said a study of subcutaneous use would continue.
Some had predicted that the IV studies of bapineuzumab would fail because they were treating those whose brains were already damaged.
“One of the strong thoughts in the field is that you really have to treat people before they become demented,” William Thies, chief scientific officer of the Alzheimer’s Association told Reuters, adding that the announcement did not prevent the drug from being tested as a preventative.
And William Thies said that despite the trial’s failure, data from the experiment could still be useful.
“These studies are terribly important for us to learn about Alzheimer’s disease, and that part of the process is just starting as the data continues to be crunched in a variety of ways.”
Johnson and Johnson had agreed in 2009 to invest up to $1.5 billion in bapineuzumab.
In a statement, Steven Romano, head of Pfizer’s Medicines Development Group said they were “obviously very disappointed” with the trial’s outcome.
“We are also saddened by the lost opportunity to provide a meaningful advance for patients afflicted with mild-to-moderate Alzheimer’s disease and their caregivers,” he said.
A similar drug being developed by Eli Lilly, solanezumab, is also considered a long-shot to succeed, but results of the trials will not be available until later this year.
A simple walking test could show if Alzheimer’s patients have the disease, say researchers after they found a link between the two.
In one test patients with a shorter stride and lower cadence and velocity in their walk also experienced memory problems and issues with cognition.
Another test found a person’s gait became “slower and more variable as cognition decline progressed”.
The findings are the first time that a physical symptom has been linked to the disease.
Previous research looked into cognition by carrying out neurological exams which tended to be costly and take a long time.

A simple walking test could show if Alzheimer’s patients have the disease
In future patients could simply be asked to walk and be observed over a number of months to see if they are at risk.
Crucially, the scientists said that walking changes can occur even before cognition decline surfaces.
Both pieces of research were presented at Alzheimer’s Association International Conference in Vancouver, Canada.
The first from the US-based Mayo Clinic involved monitoring how 1,341 participants walked through a gait sensor in two or more visits spaced 15 months apart.
The researchers found that walking changes occur because the disease interferes with the circuitry between areas of brain.
Lead researcher Rodolfo Savica said: “Walking and movements require a perfect and simultaneous integration of multiple areas of the brain.
“These changes support a possible role of gait changes as an early predictor of cognitive impairment.”
The second piece of research was carried out by Basel Mobility Center in Basel, Switzerland, and was on 1,153 adults with a mean age of 78.
The team found that people with Alzheimer’s walked more slowly than those with mild cognitive impairment.
They said that an annual test might help detect the disease early and that often relatives of Alzheimer’s patients comment on how badly a person is walking.
Bill Thies, chief medical and scientific officer for the US-based Alzheimer’s Association, said: “Monitoring deterioration and other changes in a person’s gait is ideal because it doesn’t require any expensive technology or take a lot of time to assess.”
Recent research into Alzheimer’s found that signs of dementia may appear 25 years before patients or their family sees any outward symptoms.
Scientists from Washington University School of Medicine in St Louis believe the brains and spines of those with the disease change in their 30s and 40s, several decades before memory loss and confusion sets in.
Scientists say that having regular lie-ins in old age can bring on dementia.
Getting too much or too little sleep increases your mental age by two years, researchers showed.
There is what scientists call the “goldilocks zone”, seven hours, which is neither too much nor too little.
A series of studies presented at an Alzheimer’s conference in Vancouver shows when it comes to mental decline sleep can play an important part.
It adds to evidence that poor sleep quality and quantity in the elderly increases the risk of a range of illnesses – including heart disease and diabetes.
Dr. William Thies, of the Alzheimer’s Association in the US who organized the annual meeting, said: “We know sleep patterns change as people age and that poor sleep affects overall health.
“What we don’t know for certain is whether poor sleep has long-term consequences on cognitive function.”
He said the latest research suggests cognitive health declines over the long term in some people with sleep problems.

Getting too much or too little sleep increases your mental age by two years
Dr. William Thies said: “The good news is tools already exist to monitor sleep duration and quality and to intervene to help return sleep patterns to normal.
“If we do this, there is the possibility that we may also help people preserve their cognitive health, but that needs to be tested.”
Previous studies have suggested sleep duration shorter or longer than the recommended seven hours per day may increase the risk of cardiovascular disease and type 2 diabetes.
But little research has been carried out on its affect on cognition among older individuals.
So Dr. Elizabeth Devore, of Brigham and Women’s Hospital, Boston, and colleagues followed up over 15,000 retired nurses aged 70 or older every other year for six years.
Those who slept five hours or less or nine hours or more per day had lower average cognition than those who slept seven hours.
Too little or too much sleep was cognitively equivalent to ageing by two years.
The women were recruited for the long-term study in their early 40s and those whose sleep changed by two hours per day or more in later life had worse cognitive function than those with no change, independent of their initial duration.
In a small sample of women who gave blood samples declining ratios of proteins that suggest Alzheimer’s disease brain changes were present in those who slept less or more than seven hours.
Dr. Elizabeth Devore said: “Our findings support the notion that extreme sleep durations and changes in sleep duration over time may contribute to cognitive decline and early Alzheimer’s changes in older adults.
“The public health implications of these findings could be substantial, as they might lead to the eventual identification of sleep- and circadian- based strategies for reducing risk of cognitive impairment and Alzheimer’s.”
As people age, they are more likely to develop problems with sleeping, such as insomnia, sleep apnea and disruptions in circadian rhythm that follow a 24-hour cycle.
Another five year study of 1,300 older women by California University researchers showed participants with sleep apnoea had more than twice the odds of developing dementia compared with those who did not have sleep-disordered breathing.
Women who developed a disruption of their body clock were also at increased risk of dementia and those with greater nighttime wakefulness were more likely to score worse on tests of global cognition and verbal skills.
Dr. Kristine Yaffe said: “We believe these results indicate the relationship between sleep disordered breathing and dementia may be connected to the decrease in oxygen associated with sleep apnoea and not to disrupted patterns of sleep.
“Overall, our findings support a relationship between sleep disturbances and cognitive decline in late age.
“They suggest health practitioners should consider assessing older people with sleep disorders for changes in cognition.”
She said with additional long-term research treatment of sleep disorders may be a promising method of delaying the development of dementia.
A third study of nearly 5,000 over 65 year-olds showed excessive daytime sleepiness – reported by 17.9% of participants – independently increased the risk of cognitive decline along with difficulty maintaining sleep – reported by 63.5%.
Dr. Claudine Berr, of the National Institute of Health and Medical Research in Montpellier, France, said: “These results suggest excessive daytime sleepiness may be an early predictor of cognitive decline and sleep complaints should be adequately evaluated in older persons.”
US scientists have recently identified a possible genetic link between diabetes and Alzheimer’s disease.
It has been known for some time that people with diabetes have a much higher risk of developing Alzheimer’s, but not why this is so.
Now researchers writing in Genetics say a study of worms has indicated a known Alzheimer’s gene also plays a role in the way insulin is processed.
Dementia experts said more work in humans was now needed.
US scientists have recently identified a possible genetic link between diabetes and Alzheimer's disease
Alzheimer’s is the most common cause of dementia.
There are medications which can slow the progress of the disease, but none that can halt its progress.
A key indication of Alzheimer’s, which can only be seen after death, is the presence of sticky plaques of amyloid protein in decimated portions of patients’ brains.
Scientists have already found mutations in a gene involved in the processing of amyloid protein in Alzheimer’s which run in families.
In this study, a team from the City College of New York looked at a similar gene in the nematode worms (C. elegans).
These worms are often studied because they, perhaps surprisingly, a useful model for human research.
The researchers, led by Prof. Chris Li, found the gene in the worms also affected the insulin pathway – the chemical reactions involved in its production and processing.
Prof. Chris Li said: “People with type 2 diabetes have an increased risk of dementia.
“The insulin pathways are involved in many metabolic processes, including helping to keep the nervous system healthy.”
She said more work was needed to investigate this potential link and its effects further.
Mark Johnston, editor-in-chief of the journal Genetics, said it was “an important discovery”.
“We know there’s a link between Alzheimer’s and diabetes, but until now it was somewhat of a mystery.
“This finding could open new doors for treating and preventing the disease.”
 Prev12Page 2 of 2
Prev12Page 2 of 2