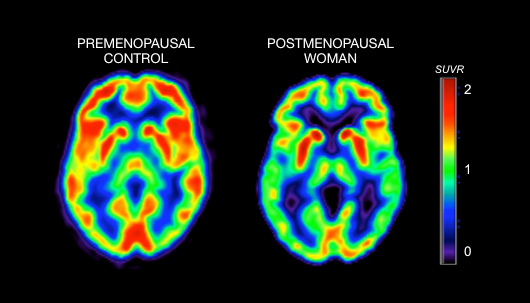
CAMBRIDGE, UK — A landmark study has revealed that the transition into menopause triggers a significant loss of gray matter in brain regions identical to those ravaged by early-stage Alzheimer’s disease, potentially solving the long-standing mystery of why women are nearly twice as likely to develop dementia as men.
The research, led by the University of Cambridge and published Tuesday in Psychological Medicine, analyzed data from more than 124,000 women. It found that the precipitous drop in estrogen during menopause acts as a “neurological shock,” accelerating the aging process in the hippocampus and entorhinal cortex—the brain’s primary centers for memory and navigation.
“The brain regions where we saw these differences are the very ones affected by Alzheimer’s,” said Professor Barbara Sahakian, the study’s senior author. “Menopause may be creating a window of vulnerability that makes women much more susceptible to neurodegeneration further down the line.”
A Structural Shift in the ‘Gateway’ to Memory
Using high-resolution MRI scans from over 11,000 participants, researchers identified a “striking” reduction in gray matter volume among post-menopausal women. Gray matter contains the nerve cell bodies essential for processing information and managing emotions.
The study highlighted three specific “at-risk” zones:
- The Hippocampus: Critical for forming and storing new memories.
- The Entorhinal Cortex: Often called the “gateway” to the brain, it is the first area typically damaged in Alzheimer’s.
- The Anterior Cingulate Cortex: Responsible for emotional regulation and decision-making.
While gray matter loss is a natural part of aging for both sexes, the researchers found that menopause accelerates this decline in women. Interestingly, while the structural changes were evident, memory performance remained stable in the short term, suggesting the brain may be “compensating” for the loss before clinical symptoms appear years later.
The HRT Debate: A Speed Bump, Not a Cure
The study also waded into the contentious debate over Hormone Replacement Therapy (HRT). Researchers found that while HRT does not appear to prevent the overall loss of brain volume, it does seem to “put the brakes” on cognitive slowing.
Women on HRT demonstrated significantly faster reaction times than those who were not, suggesting that estrogen may preserve the “processing speed” of the brain even as the structure changes.
“Reaction times naturally slow as we age,” explained Dr. Katharina Zühlsdorff, a co-author of the study. “Menopause accelerates this process, but HRT appears to slow the aging process slightly, keeping the brain’s ‘quiz-speed’ intact.”
Beyond Biology: The Mental Health Toll
The Cambridge study further confirmed that the transition is not merely a biological shift but a mental health crisis. Post-menopausal women were found to be significantly more likely to suffer from:
- Insomnia and Sleep Fragmentation: Reported across all post-menopausal groups.
- Anxiety and Depression: Leading to a higher rate of antidepressant prescriptions compared to pre-menopausal women.
- Chronic Fatigue: Paradoxically, women on HRT reported feeling the most tired, despite sleeping the same amount as their peers.
| Group | Gray Matter Volume | Reaction Speed | Mental Health Risk |
| Pre-Menopausal | High (Baseline) | Fast | Lower |
| Post-Menopause (No HRT) | Significantly Lower | Slower | Higher |
| Post-Menopause (With HRT) | Significantly Lower | Fast (Preserved) | Higher |
The ‘Critical Window’
The findings support a growing medical consensus known as the “Critical Window Hypothesis.” This suggests that the timing of estrogen loss—and the timing of medical intervention—is the key to long-term brain health.
“We can no longer view menopause as just a reproductive end-point,” said Michelle Dyson, CEO of the Alzheimer’s Society. “This study proves it is a major neurological event. We need to be screening for brain health during this period with the same urgency we use for bone density or heart health.”
As 2026 unfolds, the medical community is calling for a “precision medicine” approach to the menopause transition, urging women to focus on lifestyle factors—such as aerobic exercise and a neuroprotective diet—to build “cognitive reserve” while the brain is at its most vulnerable.