Home Tags Posts tagged with "hiv infection"
hiv infection
According to a new study published in Science Translational Medicine, a 10th of children have a “monkey-like” immune system that stops them developing AIDS.
The study found the children’s immune systems were “keeping calm”, which prevented them being wiped out.
An untreated HIV infection will kill 60% of children within two and a half years, but the equivalent infection in monkeys is not fatal.
The findings could lead to new immune-based therapies for HIV infection.
HIV eventually wipes out the immune system, leaving the body vulnerable to other infections, what is known as acquired human immunodeficiency syndrome (AIDS).
The researchers analyzed the blood of 170 children from South Africa who had HIV, had never had antiretroviral therapy and yet had not developed AIDS.
Tests showed they had tens of thousands of human immunodeficiency viruses in every milliliter of their blood.
This would normally send their immune system into overdrive, trying to fight the infection, or simply make them seriously ill, but neither had happened.
Counter-intuitively, not attacking the virus seems to save the immune system.
HIV kills white blood cells – the warriors of the immune system.
When the body’s defenses go into overdrive, even more of them can be killed by chronic levels of inflammation.
For scientists, the way the 10% of children cope with the virus has striking similarities to the way more than 40 non-human primate species cope with simian immunodeficiency virus or SIV.
They have had hundreds of thousands of years to evolve ways to tackle the infection.
This defense against AIDS is almost unique to children.
Adult humans’ immune systems tend to go all-out to finish off the virus in a campaign that nearly always ends in failure.
Children have a relatively tolerant immune system, which becomes more aggressive in adulthood – chickenpox, for example, is far more severe in adults due to the way the immune system reacts.
This does mean that as the protected children age and their immune system matures, there is a risk of them developing AIDS.
Some do, some remain AIDS-free.
People with HIV can have normal life-expectancy if they have access to antiretroviral drugs.
But their super-heated immune system never returns to normal, and they face greater risks of cardiovascular disease, cancer and dementia.
According to a United Nations AIDS report, the goal to get HIV treatment to 15 million people by the end of 2015 has already been met.
The landmark figure was reached in March – nine months ahead of schedule.
It follows decades of global efforts and investment to get antiretroviral drugs to those in need – such as people living in sub-Saharan Africa.
In 2000, when the UN first set goals to combat HIV, fewer than 700,000 people were receiving these vital medicines.
According to UNAIDS, which has a report out today, the global response to HIV has averted 30 million new HIV infections and nearly eight million AIDS-related deaths since the millennium.
Over the same time frame, new HIV infections have fallen from 2.6 million per year to 1.8 million, and AIDS-related deaths have gone down from 1.6 million to 1.2 million.
Meanwhile, global investment in HIV has gone up from $4.8 billion in 2000 to more than $20 billion in 2014.
And concerted action over the next five years could end the AIDS epidemic by 2030, says UNAIDS.
However, progress has been slower in some areas.
A major gap seems to be in awareness of HIV status, which is the biggest barrier to treatment access, says the report.
And treatment access for children has lagged behind adults – although this is now improving.
The proportion of children living with HIV who receive antiretroviral therapy almost doubled between 2010 and 2014 (from 14% to 32%), but coverage “remains notably lower than it does for adults”, says the report.
Even though new HIV infections have gone down, there is still an unacceptable number of new HIV infections each year, contributing to the burden of the epidemic.
In 2014, sub-Saharan Africa accounted for 66% of all new HIV infections. And at the last headcount, there were an estimated 25.8 million people in this region living with HIV. The estimated count for the whole world was 36.9 million.
This year sees the switch from Millennium Development Goals to broader Sustainable Development Goals.
Ban Ki-moon, Secretary General of the United Nations said: “The world has delivered on halting and reversing the AIDS epidemic.
“Now we must commit to ending the AIDS epidemic as part of the Sustainable Development Goals.”
The report says the next five years will be critical and recommends front-loading investment to “sprint” towards an ambition of ending the AIDS epidemic by 2030.
The US Centers for Disease Control (CDC) has published details of a rare case of suspected female-to-female HIV infection.
A 46-year-old woman “likely acquired” the virus during a six-month monogamous relationship with a HIV-positive woman in Texas, said the CDC.
The woman was infected with a strain that had a 98% genetic match to her partner’s.

CDC has published details of a rare case of suspected female-to-female HIV infection in Texas
The virus can be transmitted when bodily fluids come into contact with cuts, abrasions and mucus membranes.
The originally uninfected partner is said to have had a history of heterosexual relationships but none during the past 10 years.
The woman also had none of the other HIV exposure risks, including intravenous drug use.
Her partner, a 43-year-old woman, had stopped taking antiretroviral drugs in 2010.
A doctors’ report showed that two patients have been taken off their HIV drugs after bone-marrow transplants seemed to clear the virus from their bodies.
One of the patients has spent nearly four months without taking medication with no sign of the virus returning.
The team at Brigham and Women’s Hospital, in the US, caution that it is far too soon to talk about a cure as the virus could return at any point.
The findings were presented at the International AIDS Society Conference.
It is difficult to get rid of an HIV infection because it hides inside human DNA, forming untouchable “reservoirs” in body.
Anti-retroviral drugs keep the virus in check within the bloodstream – but when the drugs stop, the virus comes back.
The two men, who have not been identified, had lived with HIV for about 30 years.
They both developed a cancer, lymphoma, which required a bone-marrow transplant.
Bone marrow is where new blood cells are made and it is thought to be a major reservoir for HIV.

Two patients have been taken off their HIV drugs after bone-marrow transplants seemed to clear the virus from their bodies
After the transplant, there was no detectable HIV in the blood for two years in one patient and four in the other.
The pair came off their anti-retroviral drugs earlier this year.
One has gone 15 weeks, and the other seven, since stopping treatment, and no signs of the virus have been detected so far.
Dr. Timothy J. Henrich said the results were exciting. But he added: “We have not demonstrated cure, we’re going to need longer follow-up.
“What we can say is if the virus does stay away for a year or even two years after we stopped the treatment, that the chances of the virus rebounding are going to be extremely low.
“It’s much too early at this point to use the C-word [cure].”
It is thought that the transplanted bone marrow was initially protected from infection by the course of anti-retrovirals. Meanwhile the transplant also attacked the remaining bone marrow, which was harboring the virus.
However Dr. Timothy J. Henrich cautioned that the virus could be still be hiding inside brain tissue or the gastrointestinal track.
“If [the] virus does return, it would suggest that these other sites are an important reservoir of infectious virus and new approaches to measuring the reservoir at relevant sites will be needed to guide the development of HIV curative strategies,” he said.
Timothy Brown, also known as the “Berlin patient” is thought to be the first person cured of AIDS. He had a bone marrow transplant from a rare donor who was resistant to HIV.
The two US cases both received bone marrow from normal donors.
There was also a report of an HIV cure in a baby born in Mississippi, US. She was treated with anti-retroviral drugs at birth so it is thought the virus was cleared from the body before reservoirs were established.
It is far too early to call this a cure for HIV. And even if it was a cure, it wouldn’t be a very good one.
It is very expensive and often leads to “graft-v-host” disease. There is a 15-20% mortality rate within the first few years after the transplant.
This occurs when new immune cells produced by the graft treat the rest of the body as foreign and attack it.
The two patients in this study have replaced their regimen of anti-retroviral drugs, with those to suppress the immune system.
The procedure was carried out in these patients only because they had cancer that needed to be treated.
The real value of this research for the majority of people with HIV will come from a deeper understanding of the virus and HIV reservoirs.
[youtube _eJHMQQljpM]
An immediate treatment after HIV infection may be enough to “functionally cure” about a 10th of those diagnosed early, say researchers in France.
The researchers have been analyzing 14 people who stopped therapy, but have since shown no signs of the virus resurging.
It follows reports of a baby girl being effectively cured after very early treatment in the US.
However, most people infected with HIV do not find out until the virus has fully infiltrated the body.
The group of patients, known as the Visconti cohort, all started treatment within 10 weeks of being infected.
They stuck to a course of antiretroviral drugs for three years, on average, but then stopped.
The drugs keep the virus only in check, they cannot eradicate it from its hiding places inside the immune system.
Normally, when the drugs stop, the virus bounces back.
This has not happened in the Visconti patients. Some have been able to control HIV levels for a decade.

An immediate treatment after HIV infection may be enough to functionally cure about a 10th of those diagnosed early
Dr. Asier Saez-Cirion, from the Institute Pasteur in Paris, said: “Most individuals who follow the same treatment will not control the infection, but there are a few of them who will.”He said 5-15% of patients may be functionally cured, meaning they no longer needed drugs, by attacking the virus soon after infection.
“They still have HIV, it is not eradication of HIV, it is a kind of remission of the infection.”
Their latest study, in the journal PLoS Pathogens, analyzed what happened to the immune system of the patients.
Early treatment may limit the number of unassailable HIV hideouts that are formed. However, the researchers said it was “unclear” why only some patients were functionally cured.
However, he cautioned that many patients would be diagnosed much later than in this study.
Researchers have announced that a baby girl in the US, who was born with HIV, appears to have been cured after very early treatment with standard drug therapy.
The Mississippi child is now two-and-a-half years old and has been off medication for about a year with no signs of infection.
More testing needs to be done to see if the treatment would have the same effect on other children.
But the results could possibly lead to a cure for children with HIV.
If the girl stays healthy it would be only the world’s second reported cure.
Dr. Deborah Persaud, a virologist at Johns Hopkins University in Baltimore, presented the findings at the Conference on Retroviruses and Opportunistic Infections in Atlanta.
“This is a proof of concept that HIV can be potentially curable in infants,” she said.
In 2007, Timothy Ray Brown became the first person in the world believed to have recovered from HIV.
His infection was eradicated through an elaborate treatment for leukaemia that involved the destruction of his immune system and a stem cell transplant from a donor with a rare genetic mutation that resists HIV infection.

A baby girl in the US, who was born with HIV, appears to have been cured after very early treatment with standard drug therapy
In contrast, the case of the Mississippi baby involved a cocktail of widely available drugs already used to treat HIV infection in infants.
It suggests the treatment wiped out HIV before it could form hideouts in the body.
These so-called reservoirs of dormant cells usually rapidly re-infect anyone who stops medication, said Dr. Deborah Persaud.
The baby was born in a rural hospital where the mother had only just tested positive for HIV infection.
Because the mother had not been given any prenatal HIV treatment, doctors knew the baby was at high risk of being infected.
Researchers said the baby was then transferred to the University of Mississippi Medical Center in Jackson.
Once there, paediatric HIV specialist Dr. Hannah Gay put the baby on a cocktail of three standard HIV-fighting drugs at just 30 hours old, even before laboratory tests came back confirming the infection.
“I just felt like this baby was at higher-than-normal risk and deserved our best shot,” Dr. Hannah Gay said.
[youtube fnR_tPwFZRI]
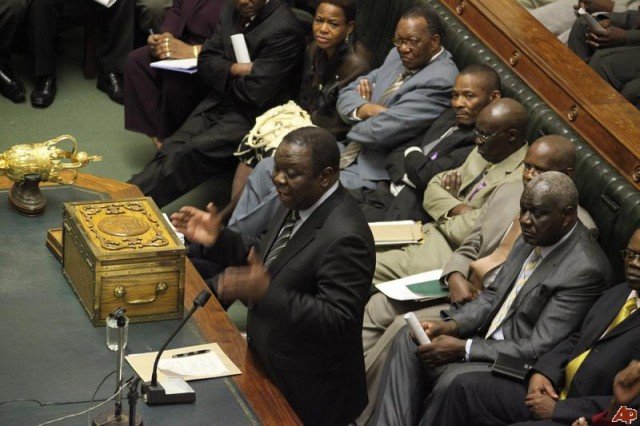
At least 10 Zimbabwean MP have been circumcised as part of a campaign to reduce HIV and AIDS cases.
A small makeshift clinic for carrying out the procedures was erected in Parliament House in the capital Harare.
Blessing Chebundo, chairman of Zimbabwe Parliamentarians Against AIDS, said his main objective was to inspire other citizens to follow suit.
Research by the UN has suggested male circumcision can reduce the spread of HIV and AIDS.
A report by UNAIDS and the World Health Organisation (WHO) said the risk of HIV infection among men could be reduced by 60%.
More than a million people in Zimbabwe are believed to be HIV-positive, with about 500,000 receiving anti-retroviral treatment.
The country was one of 13 African states identified in 2007 as a priority for the development of male circumcision programmes by the WHO and UNAIDS.
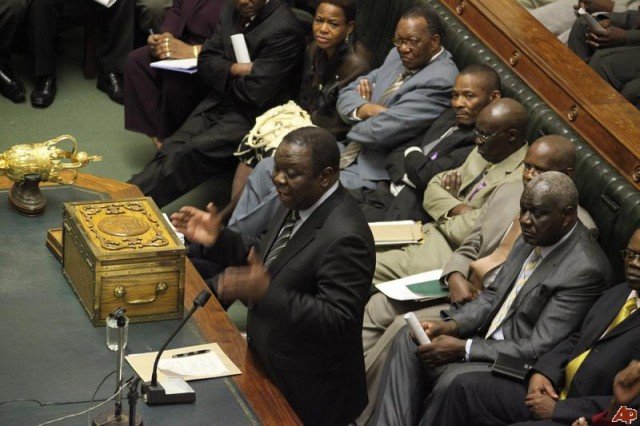
At least 10 Zimbabwean MP have been circumcised as part of a campaign to reduce HIV and AIDS cases
Blessing Chebundo said more than 120 MPs and parliamentary staff had shown an interest in the circumcision programme.
At least 10 MPs and 13 other people had the procedure performed.
Blessing Chebundo was the first to undergo the 10-minute operation.
He said there was a possibility that some members of the executive may also attend, including President Robert Mugabe.
The circumcision programme had attracted a lot of attention in Zimbabwe, and had divided opinion.
The issue was raised in parliament in September 2011, when Deputy Prime Minister Thokozani Khupe made a plea to her fellow politicians.
At the time, many MPs shunned the idea.
As well as a clinic in parliament, the initiative has seen a tent set up across the road from parliament, where counselling sessions will be held.
Dr. Owen Mugurungi, Director for AIDS and TB unit with the Ministry of Health and Child Welfare, applauded those involved, the Zimbabwe Mail reported.
“We are happy with this initiative and we are happy more leaders will come on board,” he was quoted as saying.
How circumcision may protect against HIV infection?
Specific cells in the foreskin are thought to be potential targets for HIV infection. Following circumcision, the skin under the foreskin becomes less sensitive and is less likely to bleed, reducing the risk of infection.
When AIDS first began to emerge in Africa, researchers noted that men who were circumcised seemed to be less at risk of infection, but the reasons were unclear.
Trials suggest that male circumcision could reduce the risk of HIV infection, acquired through heterosexual intercourse, by up to 60%.
The WHO says the practice is particularly effective in countries with high HIV rates.
But it is not the whole solution. Promoting safe sex, providing people with HIV testing services and encouraging the use of male and female condoms are all seen as equally important.
Some experts also say there is a danger in sending out a message that circumcision can protect against HIV because it could lead to an increase in unprotected sex.
US Antiviral Drugs Advisory Committee, which advises the FDA, has for the first time backed a drug to prevent HIV infection in healthy people.
The panel of health experts recommended US regulators approve daily pill Truvada for use by people considered at high risk of contracting the AIDS virus.
The US Food and Drug Administration (FDA) is not required to follow the panel’s advice, but it usually does.
Some health workers and groups active in the HIV community have opposed the approval of the drug.
However, the move could prove to be a new milestone in the fight against HIV/AIDS.
The Antiviral Drugs Advisory Committee recommended US regulators approve Truvada for use by people considered at high risk of contracting the AIDS virus
Truvada is already approved by the FDA for people who are HIV-positive, and is taken along with existing anti-retroviral drugs.
Studies from 2010 showed that Truvada, made by California-based Gilead Sciences, reduced the risk of HIV in healthy gay men – and among HIV-negative heterosexual partners of people who are HIV-positive – by between 44% and 73%.
The Antiviral Drugs Advisory Committee voted 19-3 in favor of prescribing the drug to the highest risk group – non-infected men who have sex with multiple male partners.
They also approved it, by majority votes, for uninfected people with HIV-positive partners and for other groups considered at risk of acquiring HIV through sexual activity.
The votes followed an 11-hour meeting of the panel in Silver Spring, Maryland, and a lengthy public comments session.
Opposition to the prospect of approving the drug is based on concerns that users could gain a false sense of security, and fears of a drug-resistant strain of HIV.
There is also concern that the high cost of Truvada could divert limited funding from more cost-effective options.
“We need to slow down. I care too much about my community not to speak my concerns,” said Joey Terrill, of the AIDS Healthcare Foundation, which campaigned against the drug’s approval.
Nurse Karen Haughey told the panel: “Truvada needs to be taken every day, 100% of the time, and my experience as a registered nurse tells me that won’t happen.
“In my eight years, not one patient that I’ve cared for has been 100% adherent.”
But others welcomed the panel’s recommendation.
“This brings us closer to a watershed for global HIV prevention efforts,” said Mitchell Warren, executive director of the AIDS Vaccine Advocacy Coalition, after the vote.
The FDA is expected to make its decision by 15 June.
UCLA scientists have found that human stem cells can be genetically engineered into “warrior” cells that fight HIV and the new cells can attack HIV-infected cells inside a living creature.
The breakthrough discovery is hoped to be the first step towards a treatment that can eradicate HIV from an infected patient.
Much HIV research focuses on vaccines or drugs that slow the virus’s progress – but this new technique could offer hope of a “cure”.
The study, published April 12 in the journal PLoS Pathogens, demonstrates for the first time that engineering stem cells to form immune cells that target HIV is effective in suppressing the virus in living tissues.
“We believe that this study lays the groundwork for the potential use of this type of an approach in combating HIV infection in infected individuals, in hopes of eradicating the virus from the body,” said lead researcher Scott G. Kitchen.
The scientists took CD8 cytotoxic T lymphocytes – the “killer” T cells that help fight infection – from an HIV-infected individual and identified the molecule which guides the T cell in recognizing and killing HIV-infected cells.

Human stem cells can be genetically engineered into “warrior” cells that fight HIV and can attack HIV-infected cells inside a tissue
However, these T cells, while able to destroy HIV-infected cells, do not exist in great enough quantities to clear the virus from the body.
So the researchers cloned the receptor and used this to genetically engineer human blood stem cells. They then placed the engineered stem cells into human thymus tissue that had been implanted in mice, allowing them to study the reaction in a living organism.
The engineered stem cells developed into a large population of mature, multi-functional HIV-specific cells that could specifically target cells containing HIV proteins.
The researchers also discovered that HIV-specific T cell receptors have to be matched to an individual in much the same way an organ is matched to a transplant patient.
In this current study, the researchers similarly engineered human blood stem cells and found that they can form mature T cells that can attack HIV in tissues where the virus resides and replicates.
They did so by using a surrogate model, the humanized mouse, in which HIV infection closely resembles the disease and its progression in humans.
In a series of tests on the mice’s peripheral blood, plasma and organs conducted two weeks and six weeks after introducing the engineered cells, the researchers found that the number of CD4 “helper” T cells – which become depleted as a result of HIV infection – increased, while levels of HIV in the blood decreased.
“We believe that this is the first step in developing a more aggressive approach in correcting the defects in the human T cell responses that allow HIV to persist in infected people,” Scott G. Kitchen said.