Home Tags Posts tagged with "alzheimer"
alzheimer
A blood test to predict the onset of Alzheimer’s disease is being under development.
Research in more than 1,000 people has identified a set of proteins in the blood which can predict the start of the dementia with 87% accuracy.
The findings, published in the journal Alzheimer’s & Dementia, will be used to improve trials for new dementia drugs.

A blood test to predict the onset of Alzheimer’s disease is being under development (photo Getty Images)
Experts warned that the test was not yet ready for doctors’ surgeries.
Research into treatments for Alzheimer’s disease has been plagued by failure. Between 2002 and 2012, 99.6% of trials aimed at preventing or reversing the disease flopped.
Doctors believe the failure is down to treating patients when it is already too late, since symptoms appear around a decade after the start of the disease.
Identifying patients earlier is one of the priorities for dementia research.
The British research group, which combines university and industry scientists, looked for differences in the blood of 452 healthy people, 220 with mild cognitive impairment and 476 with Alzheimer’s disease.
They were able to tell with 87% accuracy which patients with mild cognitive impairment would go on to develop Alzheimer’s disease in the next year.
Glen Campbell’s Alzheimer’s disease has worsened to the point where he needs full-time professional care, his wife Kim has said.
Glen Campbell, 78, revealed he had been diagnosed with the disease in 2011.
Kim Campbell said doctors had persuaded her to discontinue care at the family’s home, angering the country music star’s daughter Debby.

Glen Campbell’s Alzheimer’s disease has worsened to the point where he needs full-time professional care (photo People Magazine)
“I am his wife and no one wants him home more than me but I must do what is in his best interest,” Kim Campbell told AP.
“It is crushingly sad to see him afflicted with Alzheimer’s but indulging those feelings does not help him,” added Kim Campbell, the singer’s fourth wife of 32 years.
Talking about the care her husband is now receiving, Kim Campbell said: “He has activities and therapies to stimulate him and help him experience daily moments of success.
“His life is filled with love and laughter and he is being cared for round the clock by people who specialize in Alzheimer’s care and happen to adore him.”
Debby Campbell, one of the singer’s eight children, told Country Weekly magazine last week that she was unhappy with the decision to move her father into care.
She also said Glen Campbell had not been receiving enough attention from family members in Nashville, where the music star lives.
However, Kim Campbell countered by saying she spent time with her husband every day and that two of his children who live in Nashville visit weekly.
She also said she organized activities for the artist.
Glen Campbell issued two albums and went on a world tour following his diagnosis.
At the time, his wife said the tour was a way to help her husband combat the disease and spend time with his family members, including Debby, who was in his band and travelled with him.
Glen Campbell received a Lifetime Achievement Grammy in 2012. He has also been named Male Vocalist of the Year by the Country Music Association (CMA) and the Academy of Country Music (ACM).
In 2005, Glen Campbell was inducted into the Country Music Hall of Fame.
[youtube mizhYEEfcXo 650]
A representative for Sean Connery has strongly denied reports that the actor is suffering from Alzheimer’s after German newspaper Bild, carrying quotes from best friend Michael Caine, said that the star was “no longer in control of his senses”.
In an interview with Bild am Sonntag, Michael Caine said: “One must have serious concerns for him.”
Bild said the loss of his memory is “noticeable” and that only a few close friends and confidantes, like Michael Caine, had access to him.
“Connery forgets his life,” was the headline in the paper, Europe’s biggest selling Sunday newspaper.
The newspaper said his wife Micheline Roquebrune, 77, was always frightened to pick up the phone when he was out on the streets of Manhattan in case of bad news, suggesting Sean Connery can sometimes not find his way home.
Sean Connery’s representative has strongly denied reports that the actor is suffering from Alzheimer’s
Sean Connery, 83, told a British newspaper two years ago that he had no interest in acting any longer.
The last time Sean Connery appeared before the cameras was in 2003 for The League of Extraordinary Gentlemen.
Sean Connery and Michael Caine became friends during the shooting of the 1975 epic The Man Who Would Be King.
A spokeswoman for Sean Connery denied the claims, saying that Michael Caine had been misquoted.
“The same article also have Sean living in Spain where you all know he does not live,” the spokeswoman said.
“This [article] is truly silly and nonsense. I do not wish to give credence to this ridiculous story.”
[youtube 6GoKKgp1088]
According to a recent research, eating too much red meat could trigger Alzheimer’s disease.
Scientists found that a build-up of iron – abundant in red meat – could cause oxidant damage, to which the brain is particularly vulnerable.
Researchers say this could in turn increase the risk of Alzheimer’s.
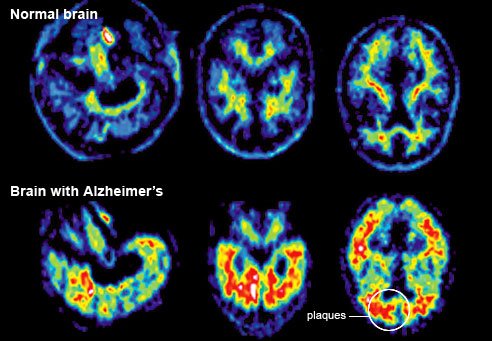
Prof. George Bartzokis of UCLA said that more studies have suggested the disease is caused by one of two proteins, one called tau, the other beta-amyloid.
As we age, most scientists say, these proteins either disrupt signaling between neurons or simply kill them.
He and colleagues looked at two areas of the brain in patients with Alzheimer’s and they compared the hippocampus, which is known to be damaged early in the disease, and the thalamus, an area that is generally not affected until the late stages.
Using brain-imaging techniques, they found that iron is increased in the hippocampus and is associated with tissue damage in that area. But increased iron was not found in the thalamus.
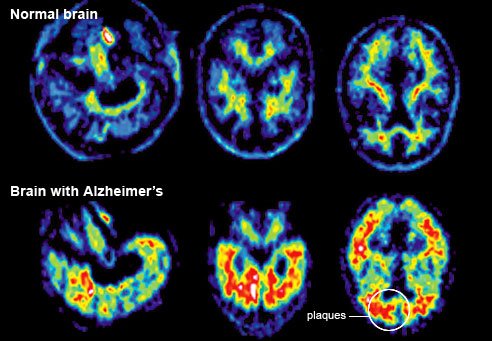
Prof. George Bartzokis said that most research had focused on the buildup of the proteins tau or beta-amyloid that cause the plaques associated with the disease.

Eating too much red meat could increase the risk of Alzheimer’s
But he believes the breakdown occurs further “upstream”, and it is the protein’s destruction of myelin, the fatty tissue which enables nerve signals to be sent along fibres, which disrupts communication and promotes the build-up of the plaques.
These amyloid plaques in turn destroy more and more myelin, disrupting brain signaling and leading to cell death and the classic clinical signs of Alzheimer’s.
He points out that myelin is produced by cells called oligodendrocytes.
These cells, along with myelin itself, have the highest levels of iron of any cells in the brain, George Bartzokis says.
He adds that although iron is essential for cell function, too much of it can promote oxidative damage, to which the brain is especially vulnerable.
Hypothesizing that elevated iron in the tissues could cause tissue breakdown, he targeted the vulnerable hippocampus, a key area of the brain involved in the formation of memories, and compared it to the thalamus, which is relatively spared by Alzheimer’s until the very late stages of disease.
They found increased iron levels in patients with Alzheimer’s.
Prof. George Bartzokis said: “It is difficult to measure iron in tissue when the tissue is already damaged.”
But the MRI technology we used in this study allowed us to determine that the increase in iron is occurring together with the tissue damage.
“We found that the amount of iron is increased in the hippocampus and is associated with tissue damage in patients with Alzheimer’s but not in the healthy older individuals – or in the thalamus.
“So the results suggest that iron accumulation may indeed contribute to the cause of Alzheimer’s disease.”
The link to iron could mean that dietary changes and surgical interventions could lower the chances of the developing the disease, he said.
He explained: “The accumulation of iron in the brain may be influenced by modifying environmental factors, such as how much red meat and iron dietary supplements we consume and, in women, having hysterectomies before menopause.”
Prof. George Bartzokis said drugs are already being developed to remove iron from tissue and the new study may allow doctors to determine who is most in need of such treatments.
US scientists have found that a lifetime of too much copper in our diets may be contributing to Alzheimer’s disease.
However, research is divided, with other studies suggesting copper may actually protect the brain.
The latest study in Proceedings of the National Academy of Sciences showed high levels of copper left the brain struggling to get rid of a protein thought to cause the dementia.
Copper is a vital part of our diet and necessary for a healthy body.
Tap water coming through copper pipes, red meat and shellfish as well as fruit and vegetables are all sources of dietary copper.
The study on mice, by a team at the University of Rochester in New York, suggested that copper interfered with the brain’s shielding – the blood brain barrier.
Mice that were fed more copper in their water had a greater build-up of the metal in the blood vessels in the brain.

A lifetime of too much copper in our diets may be contributing to Alzheimer’s disease
The team said this interfered with the way the barrier functioned and made it harder for the brain to get rid of a protein called beta amyloid.
One of the hallmarks of Alzheimer’s disease is the formation of plaques of amyloid in the dying brain.
Lead researcher Dr. Rashid Deane said: “It is clear that, over time, copper’s cumulative effect is to impair the systems by which amyloid beta is removed from the brain.”
He said that copper also led to more protein being produced: “It’s a double whammy of increased production and decreased clearance of amyloid protein.
“Copper is a very essential metal ion and you don’t want a deficiency and many nutritious foods also contain copper.”
However, he said taking supplements may be “going overboard a bit”.
Commenting on the latest findings, Chris Exley, professor of bioinorganic chemistry at Keele University in the UK, said there was “no true consensus” on the role of copper in Alzheimer’s disease.
His research on human brains reached the opposite conclusion: “In our most recent work we found evidence of lower total brain copper with ageing and Alzheimer’s. We also found that lower brain copper correlated with higher deposition of beta amyloid in brain tissue.
“He said at the moment we would expect copper to be protective and beneficial in neurodegeneration, not the instigator, but we don’t know.
“The exposure levels used mean that if copper is acting in the way they think it does in this study then it must be doing so in everyone.”
A new test could detect Alzheimer’s disease at least ten years before symptoms appear – paving the way for early treatment.
The discovery of a fall in levels of a certain type of genetic material could signal an increased risk of developing Alzheimer’s.
The biological marker is found in cerebral spinal fluid (CSF) at least 10 years before signs of dementia become apparent.
Currently, the only way to accurately diagnose the disease is by post-mortem neuropathological analysis, although memory and other brain function tests are used to determine whether drugs and other treatment may help.
Spanish researchers at the CSIC Institute of Biomedical Research of Barcelona believe they may have found a marker that could suggest the disease process is underway before symptoms start to show.

A new test could detect Alzheimer’s disease at least ten years before symptoms appear
They found a drop in the content of mitochondrial DNA (mtDNA) – genetic material present in the energy centre of cells – in spinal fluid may be a signal for the disease.
They suggest that decreased mtDNA levels reflect the diminishing ability of mitochondria to power brain cells, thus triggering their death.
The drop in the concentration of mtDNA precedes the appearance of other recognized biochemical Alzheimer’s biomarkers, suggesting the process of Alzheimer’s disease starts earlier than previously thought and that mtDNA depletion may be one of the earliest predictors.
Researchers have previously been unable to detect the genetic material in spinal fluid, but they used a new technique to amplify tiny amounts, says a study in the journal Annals of Neurology.
The researchers hope other labs and hospitals will be able to replicate the results.
The researchers say by finding a way to block the degeneration, clinicians may be able to diagnose and treat the disease before symptoms even appear.
Lead author Dr. Ramon Trullas said: “If our initial findings can be replicated by other laboratories, the results will change the way we currently think about the causes of Alzheimer’s.”
“This discovery may enable us to search for more effective treatments that can be administered during the pre-clinical stage.”
Researchers say they are closer to developing a blood test that could diagnose Alzheimer’s.
There is no definitive test for the brain-wasting disease. Doctors rely on cognition tests and brain scans.
A technique published in the journal Genome Biology showed differences in the tiny fragments of genetic material floating in the blood could be used to identify patients.
The test was accurate 93% of the time in trials on 202 people.
One of the main goals of Alzheimer’s research is to find ways of detecting the disease earlier.

Researchers say they are closer to developing a blood test that could diagnose Alzheimer’s
It starts years before symptoms appear and it is thought that future treatments will need to be given before large parts of the brain are destroyed. This will require new ways of testing for the condition.
The team at the Saarland University, in Germany, analyzed 140 microRNAs (fragments of genetic code) in patients with Alzheimer’s disease and in healthy people.
They found 12 microRNAs in the blood which were present in markedly different levels in people with Alzheimer’s. These became the basis of their test.
Early trials showed it was successful and was “able to distinguish with high diagnostic accuracies between Alzheimer’s disease patients and healthy” people.
However, more research to improve accuracy and to see whether it would work in the clinic is still needed before the test would be considered as a way of diagnosing patients.
A new study suggests that keeping mentally active by reading books or writing letters helps protect the brain in old age.
A lifetime of mental challenges leads to slower cognitive decline after factoring out dementia’s impact on the brain, US researchers say.
The study, published in Neurology, adds weight to the idea that dementia onset can be delayed by lifestyle factors.
An Alzheimer’s charity said the best way to lower dementia risk was to eat a balanced diet, exercise and stay slim.
In a US study, 294 people over the age of 55 were given tests that measured memory and thinking, every year for about six years until their deaths.

Keeping mentally active by reading books or writing letters helps protect the brain in old age
They also answered a questionnaire about whether they read books, wrote letters and took part in other activities linked to mental stimulation during childhood, adolescence, middle age, and in later life.
After death, their brains were examined for evidence of the physical signs of dementia, such as brain lesions and plaques.
The study found that after factoring out the impact of those signs, those who had a record of keeping the brain busy had a rate of cognitive decline estimated at 15% slower than those who did not.
Dr. Robert Wilson, of Rush University Medical Center in Chicago, who led the study, said the research suggested exercising the brain across a lifetime was important for brain health in old age.
He said: “The brain that we have in old age depends in part on what we habitually ask it to do in life.
“What you do during your lifetime has a great impact on the likelihood these age-related diseases are going to be expressed.”
US researchers from Washington University School of Medicine have identified genetic markers that could help highlight who is at risk of developing Alzheimer’s disease.
The research in Neuron identifies mutations that affect the build-up of certain proteins in the brain.
High levels of these tau proteins increase the chance of having the disease.

US researchers from Washington University School of Medicine have identified genetic markers that could help highlight who is at risk of developing Alzheimer’s disease
Tangles of a kind of tau called phosphorylated tau (ptau) are a hallmark of the disease.
One of the new gene variants identified by the scientists was also shown to be linked to a small increased risk of developing Alzheimer’s and a greater risk of cognitive decline.
The team used genetic information from more than 1,200 people, significantly larger than previous studies in this area.
Dr. Alison Goate, who led the study, said: “We anticipate that knowledge about the role of these genes in Alzheimer’s disease may lead to the identification of new targets from therapies or new animal or cellular models of the disease.”
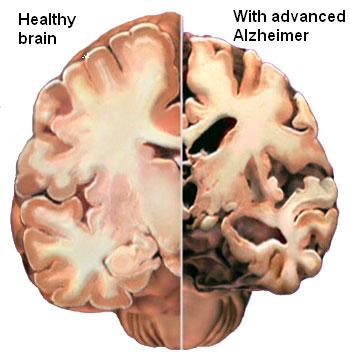
A new study has revealed that some of the earliest signs of Alzheimer’s disease have been found in the brain, more than two decades before the first symptoms usually appear.
Treating the disease early is thought to be vital in order to prevent damage to memory and thinking.
A study, published in the Lancet Neurology, found differences in the brains of people destined to develop an early form of Alzheimer’s.
Experts said the US study may give doctors more time to treat people.
Alzheimer’s disease starts long before anyone would notice; previous studies have shown an effect on the brain 10-15 years before symptoms.
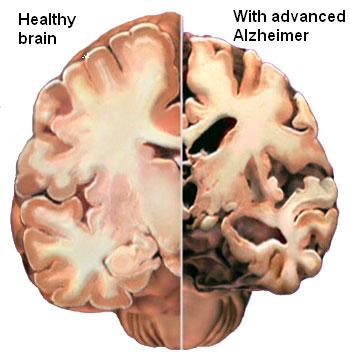
It is only after enough brain cells have died that the signs of dementia begin to appear – some regions of the brain will have lost up to 20% of their brain cells before the disease becomes noticeable.
However, doctors fear so much of the brain will have degenerated by this time that it will be too late to treat patients. The failure of recent trials to prevent further cognitive decline in patients with mild to moderate Alzheimer’s disease has been partly put down to timing.
A team at the Banner Alzheimer’s Institute in Arizona looked at a group of patients who have familial Alzheimer’s. A genetic mutation means they nearly always get the disease in their 40s. Alzheimer’s normally becomes apparent after the age of 75.
Brain scans of 20 people with the mutation, aged between 18 and 26, already showed differences compared with those from 24 people who were not destined to develop early Alzheimer’s.
The fluid which bathes the brain and spinal cord also had higher levels of a protein called beta-amyloid.
The researchers said differences could be detected “more than two decades before” symptoms would appear in these high-risk patients.
Dr. Eric Reiman, one of the scientists involved, said: “These findings suggest that brain changes begin many years before the clinical onset of Alzheimer’s disease.
“They raise new questions about the earliest brain changes involved in the predisposition to Alzheimer’s and the extent to which they could be targeted by future prevention therapies.”
Prof. Nick Fox, from the Institute of Neurology at University College London, said some of his patients had lost a fifth of some parts of their brain by the time they arrived at the clinic.
He said: “I don’t think this pushes us forwards in terms of early diagnosis, we already have markers of the disease.
“The key thing this does is open up the window of early intervention before people take a clinical and cognitive hit.”
However, he said this raised the question of how early people would need to be treated – if drugs could be found.
Dementia signs
• Struggling to remember recent events
• Problems following conversations
• Forgetting the names of friends or objects
• Repeating yourself
• Problems with thinking or reasoning
• Confusion in familiar places
Drinking a litre of mineral water every day can prevent cognitive decline in Alzheimer’s sufferers by removing aluminium from their bodies, a new study has found.
British researchers found drinking silicon-rich mineral water “significantly reduced” the levels of neurotoxin aluminium in the body.
Aluminium has long been linked to the development of Alzheimer’s but no scientific relationship has yet been proved.
Patients who took part in the new study drank a litre of mineral water every day for 13 weeks – and the majority showed no further signs of cognitive decline.
One patient saw the amount of aluminium in their body drop by 70% and three participants actually showed an improvement in their mental health.
Professor Christopher Exley, of Keele University, who led the research, said the “surprising” results gave hope to findings ways to combat the devastating disease.
He said: “There were two parts to our research. The first is that drinking silicon water does remove aluminium from the body.
“When you drink silicon-rich mineral water aluminium throughout the body is gathered up into the blood and then excreted through the urine.
“It seems to purge the aluminium from the body. We now know we can use this silicon-rich <<therapy>> water to reduce aluminium.
“The second part of our research was looking at the cognitive abilities of people with Alzheimer’s and whether these changed as the aluminium was reduced.
“The most interesting thing was that we did see this potential relationship between the removal of aluminium and the positive improvement in cognitive function.
“It is highly unlikely to see changes over such a short period of time so the fact we saw changes in cognitive ability was quite a surprise.
“We saw improvement in some cases, cognitive function remained the same in others and it did decrease in others.”
Previous studies have linked the presence of aluminium with plaques and tangles – two kinds of microscopic damage – in the brains of people with Alzheimer’s disease.
Researchers examined the aluminium levels of 15 sufferers and their carers or partners – 15 women and 15 men in total.
The brand of water used in the study – published in the Journal of Alzheimer’s Disease – was a Malaysian water called Spritzer, which has high levels of the chemical element silicon.
Brands with similar levels include Volvic and Fiji water.
Scientists asked the participants to drink a litre of Spritzer water every day for 13 weeks and measured their aluminium levels at the end.
The patients saw a huge reduction in their aluminium levels, with a number showing drops of 50, 60 and 70%.
Participants were also assessed using the ADAS-Cog (Alzheimer Disease Assessment Scale-Cognitive) method, which is a recognized 11-part test.
The tests include memory questions and “simple” tasks such as drawing a clock face – people with a deteriorating function may struggle to put the numbers in the right place.
After 13 weeks, cognitive function is eight of the 15 Alzheimer’s sufferers had not deteriorated – and actually improved “substantially” in three.
Prof. Christopher Exley added: “We now want to carry out further research to see if we could reduce the risk of Alzheimer’s who seem to be predisposed to it.
“They are usually aged between 40 and 60. If we could get people to include silicon-rich water in their diet in the future and reduce their risk, it would be a great.”
The Spritzer mineral water containing 35 mg of silicon per litre.
However, Prof. Christopher Exley says mineral water brands also contain high levels of silicon.
He said: “Volvic has high levels of silicon, around 20mg/litre. Fiji water has approximately 45mg/litre.
“There is a simple equation you can do to work out the silicon levels in water. If you look at the back of the bottle, it will often state a mg/litre analysis.
“On that list should be <<silica>>, which is silicon with oxygen. If you divide that number by two you get the approximate value of silicon in that water.”
Prof. Christopher Exley added that it is more effective to drink the water over a shorter period, such as an hour, rather than sipping it all at once, in order to remove aluminium.
“The major challenge is that we don’t have an effective drug for Alzheimer’s. This is a real tragedy,” he said.
“While we know a huge amount, we don’t have an effective drug and I think anything that shows some promise should stand a chance of being investigated.
“I think this deserves a chance.”
The research is published in the Journal of Alzheimer’s Disease Volume 33, No. 2.
A bad sleep may be an early sign of Alzheimer’s if a study in mice also applies to people, say researchers.
Clumps of protein, called plaques, in the brain are thought to be a key component of the illness.
A study, published in the journal Science Translational Medicine, showed that when plaques first developed, the mice started having disrupted sleep.
The hunt for early hints that someone is developing Alzheimer’s is thought to be crucial for treating the disease.

A bad sleep may be an early sign of Alzheimer's if a study in mice also applies to people
People do not show problems with their memory or clarity of thought until very late on in the disease. At this point, parts of the brain will have been destroyed, meaning treatment will be very difficult or maybe even impossible.
It is why researchers want to start early, years before the first symptoms.
One large area of research is in plaques of beta amyloid which form on the brain.
Levels of the beta amyloid protein naturally rise and fall over 24 hours in both mice and people. However, the protein forms permanent plaques in Alzheimer’s disease.
Experiments at Washington University showed that nocturnal mice slept for 40 minutes during every hour of daylight. However, as soon brain plaques started to form the mice were sleeping for only 30 minutes.
One of the researchers, Prof. David Holtzman, said: “If sleep abnormalities begin this early in the course of human Alzheimer’s disease, those changes could provide us with an easily detectable sign of [the disease].”
“If these sleep problems exist, we don’t yet know exactly what form they take, reduced sleep overall or trouble staying asleep or something else entirely.”
However, findings in mice do not always apply to people are there are many reasons for disrupted sleep.
US pharmaceutical companies Pfizer and Johnson & Johnson say they will stop development of Alzheimer’s drug bapineuzumab, because it failed in two late-stage clinical trials.
Bapineuzumab, made by Pfizer and Johnson & Johnson, was designed to halt build-up of plaque in the brain.
But it failed to improve cognitive or functional performance compared with a placebo in certain patients.
Alzheimer’s is the most common form of dementia, as well as the sixth leading cause of death in the United States.
An estimated 36 million people worldwide are believed to have dementia, including Alzheimer’s.

Bapineuzumab, made by Pfizer and Johnson & Johnson, was designed to halt build-up of plaque in the brain
Both firms announced on 23 July that the first clinical trial of the intravenous (IV) version of bapineuzumab had failed.
In that study, patients with a gene that is associated with a greater risk of Alzheimer’s were tested.
But results with the group were largely the same as with those who did not have the gene, who were tested in the second study.
The second trial’s end means that additional studies on the IV version will not take place; however, Johnson and Johnson said a study of subcutaneous use would continue.
Some had predicted that the IV studies of bapineuzumab would fail because they were treating those whose brains were already damaged.
“One of the strong thoughts in the field is that you really have to treat people before they become demented,” William Thies, chief scientific officer of the Alzheimer’s Association told Reuters, adding that the announcement did not prevent the drug from being tested as a preventative.
And William Thies said that despite the trial’s failure, data from the experiment could still be useful.
“These studies are terribly important for us to learn about Alzheimer’s disease, and that part of the process is just starting as the data continues to be crunched in a variety of ways.”
Johnson and Johnson had agreed in 2009 to invest up to $1.5 billion in bapineuzumab.
In a statement, Steven Romano, head of Pfizer’s Medicines Development Group said they were “obviously very disappointed” with the trial’s outcome.
“We are also saddened by the lost opportunity to provide a meaningful advance for patients afflicted with mild-to-moderate Alzheimer’s disease and their caregivers,” he said.
A similar drug being developed by Eli Lilly, solanezumab, is also considered a long-shot to succeed, but results of the trials will not be available until later this year.
A simple walking test could show if Alzheimer’s patients have the disease, say researchers after they found a link between the two.
In one test patients with a shorter stride and lower cadence and velocity in their walk also experienced memory problems and issues with cognition.
Another test found a person’s gait became “slower and more variable as cognition decline progressed”.
The findings are the first time that a physical symptom has been linked to the disease.
Previous research looked into cognition by carrying out neurological exams which tended to be costly and take a long time.

A simple walking test could show if Alzheimer’s patients have the disease
In future patients could simply be asked to walk and be observed over a number of months to see if they are at risk.
Crucially, the scientists said that walking changes can occur even before cognition decline surfaces.
Both pieces of research were presented at Alzheimer’s Association International Conference in Vancouver, Canada.
The first from the US-based Mayo Clinic involved monitoring how 1,341 participants walked through a gait sensor in two or more visits spaced 15 months apart.
The researchers found that walking changes occur because the disease interferes with the circuitry between areas of brain.
Lead researcher Rodolfo Savica said: “Walking and movements require a perfect and simultaneous integration of multiple areas of the brain.
“These changes support a possible role of gait changes as an early predictor of cognitive impairment.”
The second piece of research was carried out by Basel Mobility Center in Basel, Switzerland, and was on 1,153 adults with a mean age of 78.
The team found that people with Alzheimer’s walked more slowly than those with mild cognitive impairment.
They said that an annual test might help detect the disease early and that often relatives of Alzheimer’s patients comment on how badly a person is walking.
Bill Thies, chief medical and scientific officer for the US-based Alzheimer’s Association, said: “Monitoring deterioration and other changes in a person’s gait is ideal because it doesn’t require any expensive technology or take a lot of time to assess.”
Recent research into Alzheimer’s found that signs of dementia may appear 25 years before patients or their family sees any outward symptoms.
Scientists from Washington University School of Medicine in St Louis believe the brains and spines of those with the disease change in their 30s and 40s, several decades before memory loss and confusion sets in.
Scientists say that having regular lie-ins in old age can bring on dementia.
Getting too much or too little sleep increases your mental age by two years, researchers showed.
There is what scientists call the “goldilocks zone”, seven hours, which is neither too much nor too little.
A series of studies presented at an Alzheimer’s conference in Vancouver shows when it comes to mental decline sleep can play an important part.
It adds to evidence that poor sleep quality and quantity in the elderly increases the risk of a range of illnesses – including heart disease and diabetes.
Dr. William Thies, of the Alzheimer’s Association in the US who organized the annual meeting, said: “We know sleep patterns change as people age and that poor sleep affects overall health.
“What we don’t know for certain is whether poor sleep has long-term consequences on cognitive function.”
He said the latest research suggests cognitive health declines over the long term in some people with sleep problems.

Getting too much or too little sleep increases your mental age by two years
Dr. William Thies said: “The good news is tools already exist to monitor sleep duration and quality and to intervene to help return sleep patterns to normal.
“If we do this, there is the possibility that we may also help people preserve their cognitive health, but that needs to be tested.”
Previous studies have suggested sleep duration shorter or longer than the recommended seven hours per day may increase the risk of cardiovascular disease and type 2 diabetes.
But little research has been carried out on its affect on cognition among older individuals.
So Dr. Elizabeth Devore, of Brigham and Women’s Hospital, Boston, and colleagues followed up over 15,000 retired nurses aged 70 or older every other year for six years.
Those who slept five hours or less or nine hours or more per day had lower average cognition than those who slept seven hours.
Too little or too much sleep was cognitively equivalent to ageing by two years.
The women were recruited for the long-term study in their early 40s and those whose sleep changed by two hours per day or more in later life had worse cognitive function than those with no change, independent of their initial duration.
In a small sample of women who gave blood samples declining ratios of proteins that suggest Alzheimer’s disease brain changes were present in those who slept less or more than seven hours.
Dr. Elizabeth Devore said: “Our findings support the notion that extreme sleep durations and changes in sleep duration over time may contribute to cognitive decline and early Alzheimer’s changes in older adults.
“The public health implications of these findings could be substantial, as they might lead to the eventual identification of sleep- and circadian- based strategies for reducing risk of cognitive impairment and Alzheimer’s.”
As people age, they are more likely to develop problems with sleeping, such as insomnia, sleep apnea and disruptions in circadian rhythm that follow a 24-hour cycle.
Another five year study of 1,300 older women by California University researchers showed participants with sleep apnoea had more than twice the odds of developing dementia compared with those who did not have sleep-disordered breathing.
Women who developed a disruption of their body clock were also at increased risk of dementia and those with greater nighttime wakefulness were more likely to score worse on tests of global cognition and verbal skills.
Dr. Kristine Yaffe said: “We believe these results indicate the relationship between sleep disordered breathing and dementia may be connected to the decrease in oxygen associated with sleep apnoea and not to disrupted patterns of sleep.
“Overall, our findings support a relationship between sleep disturbances and cognitive decline in late age.
“They suggest health practitioners should consider assessing older people with sleep disorders for changes in cognition.”
She said with additional long-term research treatment of sleep disorders may be a promising method of delaying the development of dementia.
A third study of nearly 5,000 over 65 year-olds showed excessive daytime sleepiness – reported by 17.9% of participants – independently increased the risk of cognitive decline along with difficulty maintaining sleep – reported by 63.5%.
Dr. Claudine Berr, of the National Institute of Health and Medical Research in Montpellier, France, said: “These results suggest excessive daytime sleepiness may be an early predictor of cognitive decline and sleep complaints should be adequately evaluated in older persons.”
A team at Washington University School of Medicine has assembled a “timeline” of the unseen progress of Alzheimer’s before symptoms appear.
Scientists looked at families with a genetic risk of the disease.
Writing in the New England Journal of Medicine, they say signs appeared up to 25 years before the expected onset of the disease.
The 128 people in the study, from the UK, US and Australia, had a 50% chance of inheriting one of three mutations that are certain to cause early Alzheimer’s, which often develops in people’s 30s and 40s – much earlier than the more common form of Alzheimer’s which generally affects people in their 60s.
A team at Washington University School of Medicine has assembled a "timeline" of the unseen progress of Alzheimer's before symptoms appear
Those who carry the mutations will go on to develop the disease.
The researchers looked at the age the participants’ parents were when they developed the disease – and therefore how many years it was likely to be before they too showed symptoms.
They underwent blood and spinal fluid tests as well as brain scans and mental ability assessments.
The earliest change – a drop in spinal fluid levels of the key ingredient of Alzheimer’s brain plaques – can be detected 25 years before the anticipated age of disease onset, they suggest.
At 15 years, raised levels of tau, a structural protein in brain cells can be seen in spinal fluid – and shrinkage can also be detected within parts of the brain.
Changes in the brain’s use of the sugar glucose and slight memory problems become apparent 10 years before symptoms would appear, they suggest.
Researchers also tested other members of the families without the inherited mutations – and found no changes in the markers they tested for.
US scientists have recently identified a possible genetic link between diabetes and Alzheimer’s disease.
It has been known for some time that people with diabetes have a much higher risk of developing Alzheimer’s, but not why this is so.
Now researchers writing in Genetics say a study of worms has indicated a known Alzheimer’s gene also plays a role in the way insulin is processed.
Dementia experts said more work in humans was now needed.
US scientists have recently identified a possible genetic link between diabetes and Alzheimer's disease
Alzheimer’s is the most common cause of dementia.
There are medications which can slow the progress of the disease, but none that can halt its progress.
A key indication of Alzheimer’s, which can only be seen after death, is the presence of sticky plaques of amyloid protein in decimated portions of patients’ brains.
Scientists have already found mutations in a gene involved in the processing of amyloid protein in Alzheimer’s which run in families.
In this study, a team from the City College of New York looked at a similar gene in the nematode worms (C. elegans).
These worms are often studied because they, perhaps surprisingly, a useful model for human research.
The researchers, led by Prof. Chris Li, found the gene in the worms also affected the insulin pathway – the chemical reactions involved in its production and processing.
Prof. Chris Li said: “People with type 2 diabetes have an increased risk of dementia.
“The insulin pathways are involved in many metabolic processes, including helping to keep the nervous system healthy.”
She said more work was needed to investigate this potential link and its effects further.
Mark Johnston, editor-in-chief of the journal Genetics, said it was “an important discovery”.
“We know there’s a link between Alzheimer’s and diabetes, but until now it was somewhat of a mystery.
“This finding could open new doors for treating and preventing the disease.”